Fertility treatments
"Once you have undergone basic investigations your doctor may prescribe fertility treatment if you have still not managed to conceive naturally."
Once you have undergone basic investigations your doctor may prescribe fertility treatment if you have still not managed to conceive naturally. These may include: ovulation induction, intrauterine insemination or invitro-fertilisation.
OVULATION INDUCTION
Is often prescribed if you are not ovulation however sometimes it may be offered as an initial treatment prior to moving onto more involved treatment such as IVF.
Clomiphene citrate
This is most often used for women with polycystic ovarian syndrome - 60% of women with PCOS will ovulate and 40% will become pregnant whilst using clomid. It rarely works in women with hypothalamic amenorrhoea - patients with this are better to use gonadotropins. Comiphene comes in tablet form at a dose of 50mg. Patients start taking on day 2 to day 5 of their cycle sometimes a period may need to be induced by taking a progesterone tablet. It is an anti oestrogen that binds to the pituitary gland making the pituitary gland believe there is no oestrogen in your body so the pituitary gland responds by producing FSH (and LH). FSH then increase to stimulate follicular growth and the oestrogen increases and signals to the pituitary gland to have a LH surge which results in ovulation. As clomiphene increases the FSH production the ovary may produce more oocytes than one. There is a 10% risk of twins and 1% risk of high order multiples whilst taking clomiphene citrate. Clomiphene also has many side-effects: such as causing a thin endometrial lining, change to cervical mucus making it less receptive to conception, mood changes, depression, ovarian cysts, ectopic pregnancy, bloating, nausea, vomiting, visual disturbance and ovarian hyper stimulation syndrome. When your doctor prescribes this medication they should give you a pamphlet describing the possible effects.
Gonadotropins
Gonadotropins are produced by the pituitary gland. Follicle stimulating hormone is the commonly used hormone to induce follicular development. It comes in injection form and often administered in a pen form for easy use. It often causes multi- follicle development which results in a number of eggs grow. Patients taking this medication will need close monitoring with bloods and ultrasounds. Occasionally patients will over respond and will need to be cancelled. When the follicles have reached maturity it is usually when they reach 16mm or over your doctor will administer a trigger shot of HCG that will release the egg/eggs. Ovulation will occur usually between 36-40 hours post trigger injection. Your doctor will advise you to have intercourse the day after your trigger and 2 days after or they may advise an insemination.
INTRA-INSEMNATION
This is a procedure where the sperm is centrifuged and washed to remove debris and prostaglandins. The sperm is then drawn up into a syringe that is then transferred into the uterus via a small catheter. To have this procedure you will need to be able to tolerate vaginal examination with speculums. There may be some uterine cramping when the catheter is placed into the uterus. The sperm will not fall out when you stand up and there is no need to go home and lie down however I recommend limiting high impact exercise post insemination.
INVITRO-FERTILISATION (IVF)
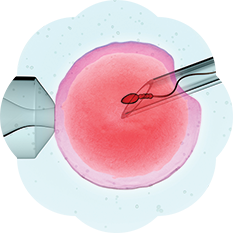
IVF is a process where oocytes and sperm fertilise outside the body the body to make embryos that are then transferred back to the female. It involves taking follicle-stimulating hormone to create between 10-15 oocytes. Some patients may over or under respond to the medication and this may need adjusting by your fertility specialist to maximise your treatment outcome. The oocytes are collected while you are sedated using vaginal probe and a need to collect the eggs. The procedure is very simple but complications can occur such as bleeding, infection and damage to internal organs. The oocytes are then transferred to the embryology lab to be fertilised with the sperm. Some couples will need intra-cytoplasmic-sperm injection (ICSI) to fertilise the oocytes. This is where the sperm is injected into the oocytes with a tiny glass pipelle. It is expected with standard and ICSI that 70% of oocytes should fertilise.
Once the embryos are made they are incubated – embryo transfer may occur on day 2,3 or day 5. Day 5 embryos are called blastocysts. To grow your embryos to blastocyst stage the embryo requires a sequential media to try and match nutrients available to the embryo in the fallopian tube. Blastocysts result in higher pregnancy rates and less chance of miscarrying. Before you commence treatment you should check that your clinic is experience at blastocyst transfer. If you have 4 or more fertilised oocytes that are of good quality then you should be able to transfer your embryos at this stage.
The embryo transfer involves insertion of a speculum into the vagina and then a tiny catheter is inserted into the uterus to deposit the embryo. This should be done under ultrasound guidance to ensure correct placement of the embryo. The embryo transfer can be done whilst you are awake or under sedation. After the transfer the embryo won’t fall out and there is no clear-cut evidence that lying in bed will help improve pregnancy rates.
PREGNANCY RATES
Clinics will offer different treatments and pregnancy rates. Please check the Infertility Treatment Authority Website to see what pregnancy rates your clinic offers. If your first cycle fails don’t be too disheartened - it may take 3-4 stimulated cycles before conception occurs occasionally sometimes longer. After your first cycle your infertility specialist may adjust your treatment to maximize your chances to conceive. Sometimes you may need additional treatments such as aspirin, steroids or heparin/clexane but this will depend on additional testing to assess for an implantation disorder.